ASSESSMENT OF RENAL AND HEPATIC DYSFUNCTION AMONG TYPHOID FEVER PATIENTS IN BINGHAM UNIVERSITY TEACHING HOSPITAL, JOS, NIGERIA: A RETROSPECTIVE STUDY
DOI:
https://doi.org/10.33003/Keywords:
Typhoid fever, Salmonella typhi, Liver dysfunction, Kidney dysfunction, sanitary infrastructureAbstract
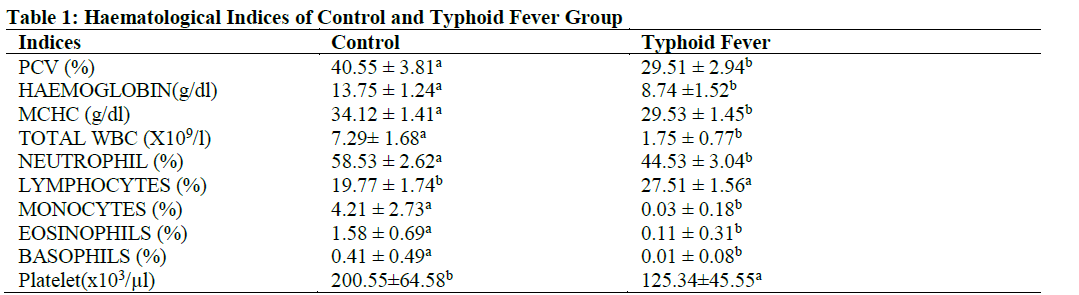
Typhoid fever-induced organ dysfunction contributes greatly to high morbidity and mortality associated with the disease. It is crucial to monitor all affected organs during treatment to improve patients’ survival. This retrospective study was conducted to evaluate the impact of typhoid fever on hepatic and renal functions among patients who attended Bingham University Teaching Hospital between 2019 and 2020. Records of 300 patients comprising 150 confirmed typhoid cases through widal test and blood culture, and 150 healthy controls were analysed. Results showed that typhoid fever resulted in severe anaemia, elevated serum liver enzymes and thrombocytopenia, however, significant alterations were more severe in male patients compared to females. Significant reduction in serum glucose levels, total white blood cell and differential white blood counts except lymphocyte counts were observed in typhoid fever patients. Although there was non-significant decrease in serum albumin and total protein of the patients, gender-specific analysis revealed a significant increase in serum albumin among female patients in contrast to male patients that exhibited a significant decrease in serum albumin. There were no significant differences in renal function parameters between the patient and the control except serum urea. In conclusion, hepatic dysfunction, severe anaemia and thrombocytopenia are strongly associated with typhoid fever in this population with the severity more pronounced among male patients compared to females, while renal impairment is relatively uncommon. It is advisable that patients in this area undergo liver and kidney function assessment in addition to their treatment to facilitate early detection of typhoid-induced hepatic and renal damage.
References
Abd-Alrazaq, F. S., & Ali, S. J. (2017). A study of the Biochemical and Haematological parameters in Patients of Typhoid Fever. Diyala J For Pure Sci, 13. https://doi.org/10.13140/RG.2.2.16689.79208
Abdulkarim, I. A., Zakari, N., & Yakudima, I. (2023). Spatio-Temporal Analysis of Typhoid Fever Mortality in Kano State, Nigeria. FUDMA J of Sci, 2(4), 113-124. https://fjs.fudutsinma.edu.ng/index.php/fjs/article/view/1326
Ahmad, M. M., Umar, U. Z., Abdullahi, I. I., Mukhtar, I. H., & Isa, S. (2023). Detection of Salmonella species among patients with suspected cases of typhoid fever in Wudil General Hospital. FUDMA J of Sci, 3(3),535-539. https://fjs.fudutsinma.edu.ng/index.php/fjs/article/view/1600
Ahmed, A.S & Ahmed, B. (2010). Jaundice in typhoid patients: differentiation from other common causes of fever and jaundice in the tropics. Ann Afr Med, 9(3), 135-140. https://doi.org/10.4103/1596-3519.68361
Al-Dahhan N. A., Hussein, B. J., & Issa, H. I. (2020). Assessment of Liver Enzymes and Cytokines in Typhoid Fever. Sys Rev Pharm, 11(3): 297 300. https://dx.doi.org/10.5530/srp.2020.3.34
Anusuya B. & Sumathi S. (2015). Haematological Alterations due to Typhoid Fever in Mayiladuthurai area, Nagapattinam. Int J of R Pharmacol & Pharmacother, 4(2): 210 - 216. https://doi.org/10.61096/ijrpp.v4.iss2.2015.210-216
Atata, J. A., Osho, B. O., Ajadi, A. A., Adam, M., & Jegede, H. O. (2025). Post-exertion Cascade: Decoding the Haemato-Biochemical Indices of Dehydration in Elite Horses. FUDMA J of Sci, 9(9), 347-352. https://doi.org/10.33003/fjs-2025-0909-3816
Butt, M. H., Saleem, A., Javed, S. O., Ullah, I., Rehman, M. U., Islam, N., . . . Misbah, S. (2021). Rising XDR-Typhoid Fever Cases in Pakistan: Are We Heading Back to the Pre-antibiotic Era? Front Public Health, 9, 794868. https://doi.org/10.3389/fpubh.2021.794868
Crawford, R. W., Rosales-Reyes, R., Ramírez-Aguilar Mde, L., Chapa-Azuela, O., Alpuche-Aranda, C., & Gunn, J. S. (2010). Gallstones play a significant role in Salmonella spp. gallbladder colonization and carriage. Proc Natl Acad Sci U S A, 107(9), 4353-4358. https://doi.org/10.1073/pnas.1000862107
Cruz Espinoza, L. M., McCreedy, E., Holm, M., Im, J., Mogeni, O. D., Parajulee, P., . . . Marks, F. (2019). Occurrence of Typhoid Fever Complications and Their Relation to Duration of Illness Preceding Hospitalization: A Systematic Literature Review and Meta-analysis. Clin Infect Dis, 69(Suppl 6), S435-s448. https://doi.org/10.1093/cid/ciz477
Darton, T,C., Blohmke, C.J,, Giannoulatou, E., Waddington, C.S., Jones, C., Sturges, P., Webster, C., Drakesmith, H., Pollard, A.J. & Armitage, A.E. Rapidly Escalating epcidin and Associated Serum Iron Starvation are Features of the Acute Response to Typhoid Infection in Humans. PLoS Negl Trop Dis. 2015 Sep 22;9(9):e0004029.
https://doi.org/10.1371/journal.pntd.0004029
de Andrade, D. R., & de Andrade Júnior, D. R. (2003). Typhoid fever as cellular microbiological model. Rev Inst Med Trop Sao Paulo, 45(4), 185-191. https://doi.org/10.1590/s0036-46652003000400002
Don, B.R. & Kaysen, G. (2004). Serum albumin: relationship to inflammation and nutrition. Semin Dial, 17(6):432-7. https://doi.org/10.1111/j.0894-0959.2004.17603.x
Erhuotor, E. E., Eggon, H. A., Ajidani, M. S., & Osekweyi, J. O. (2023). Typhoid and cholera chronicles: their dual effect on life expectancy in delta state, nigeria. FUDMA J of Sci, 7(5), 348-355. https://doi.org/10.33003/fjs-2023-0705-2028
Faruku, A., Sarkinfada, F., Taysir, R. H., Magaji, U. F., Idris, A. K., & Musa, S., (2024). Socio-demographic factors affecting the prevalence of typhoid fever among febrile patientsin Kebbi State, Nigeria. Dutse Journal of Pure and Applied Sciences, 10(1C), 263–274. https://dx.doi.org/10.4314/dujopas.v10i1c.25
Ganz, T. (2009). Iron in innate immunity: starve the invaders. Curr Opin Immunol 21: 63–67. https://doi.org/10.1016/j.coi.2009.01.011
Garrett, D. O., Longley, A. T., Aiemjoy, K., Yousafzai, M. T., Hemlock, C., Yu, A. T., . . . Luby, S. P. (2022). Incidence of typhoid and paratyphoid fever in Bangladesh, Nepal, and Pakistan: results of the Surveillance for Enteric Fever in Asia Project. Lancet Glob Health, 10(7), e978-e988. https://doi.org/10.1016/s2214-109x(22)00119-x
Haleem, N., Siddique, A. N., & Ibrar Alam, W. M. (2017). Assessment of liver function in malaria, typhoid and dengue diseases in Peshawar, Pakistan. J Entomol Zool Stud ;5(5):983-986.
Hayashi, M., Kouzu, H., Nishihara, M., Takahashi, T., Furuhashi, M., Sakamoto, K., . . . Shikano, Y. (2005). Acute renal failure likely due to acute nephritic syndrome associated with typhoid fever. Intern Med, 44(10), 1074-1077. https://doi.org/10.2169/internalmedicine.44.1074
Hu, B., Hou, P., Teng, L., Miao, S., Zhao, L., Ji, S., . . . Yue, M. (2022). Genomic Investigation Reveals a Community Typhoid Outbreak Caused by Contaminated Drinking Water in China, 2016. Front Med (Lausanne), 9, 753085. https://doi.org/10.3389/fmed.2022.753085
Ifeanyi, O. E. (2014). Changes in some haematological parameters in typhoid patients attending University Health Services Department of Michael Okpara University of Agriculture, Nigeria. Int. J. Curr. Microbiol. App. Sci, 3(1), 670-674.
Janssen van Doorn, K., Pierard, D., & Spapen, H. (2006). Acute renal dysfunction in salmonella gastroenteritis. J Clin Gastroenterol, 40(10), 910-912. https://doi.org/10.1097/01.mcg.0000212620.20079.34
Kakaria, A., Asgaonkar, D., & Narkhede, M. (2014). Clinical profile of enteric fever: A prospective study of fifty enteric fever patients. Int J Res Med Sci, 2, 1620-1625. DOI: 10.5455/2320-6012.ijrms20141170
Khan, F. Y., Al-Ani, A., & Ali, H. A. (2009). Typhoid rhabdomyolysis with acute renal failure and acute pancreatitis: a case report and review of the literature. Int J Infect Dis, 13(5), e282-285. https://doi.org/10.1016/j.ijid.2008.11.009
Khan, M., Coovadia, Y., & Sturm, A. W. (1998). Typhoid fever complicated by acute renal failure and hepatitis: case reports and review. Am J Gastroenterol, 93(6), 1001-1003. https://doi.org/10.1111/j.1572-0241.1998.298_y.x
Khanam, F., Ross, A. G., McMillan, N. A. J., & Qadri, F. (2022). Toward Typhoid Fever Elimination. Int J Infect Dis, 119, 41-43. https://doi.org/10.1016/j.ijid.2022.03.036
Khosla, S. N., Anand, A., Singh, U., & Khosla, A. (1995). Haematological profile in typhoid fever. Trop Doct, 25(4), 156-158. https://doi.org/10.1177/004947559502500404
Khosla, S. N., Singh, R., Singh, G. P., & Trehan, V. K. (1988). The spectrum of hepatic injury in enteric fever. Am J Gastroenterol, 83(4), 413-416.
Kim, C. L., Cruz Espinoza, L. M., Vannice, K. S., Tadesse, B. T., Owusu-Dabo, E., Rakotozandrindrainy, R., . . . Marks, F. (2022). The Burden of Typhoid Fever in Sub-Saharan Africa: A Perspective. Res Rep Trop Med, 13, 1-9. https://doi.org/10.2147/rrtm.S282461
Leung, D. T., Bogetz, J., Itoh, M., Ganapathi, L., Pietroni, M. A., Ryan, E. T., & Chisti, M. J. (2012). Factors associated with encephalopathy in patients with Salmonella enterica serotype Typhi bacteremia presenting to a diarrheal hospital in Dhaka, Bangladesh. Am J Trop Med Hyg, 86(4), 698-702. https://doi.org/10.4269/ajtmh.2012.11-0750
Lokhandwala, A., Athar, S., & Turrin, N. (2012). Role of absolute eosinopenia as marker of enteric fever: experience from a tertiary care hospital in the United Arab Emirates. Ibnosina Journal of Medicine and Biomedical Sciences, 4(06), 249-253. DOI: https://doi.org/10.4103/1947-489X.210782
Magaji A. & Mahmud Z. (2025), Malaria and Typhoid Co-infection among Patients Attending Health Facilities in Bauchi North, Bauchi State Nigeria Dutse J of Pure and Applied Sci (DUJOPAS), 11(1b), 66-74. https://doi.org/10.4314/dujopas.v11i1b.8
Magaji,A., Maradun R. S., Mahmud, Z., Adamu Yakubu,A., Wada G., Salim Aminu, S., & Aminu, S. (2025). The Impact of Socioeconomic and Environmental Conditions on Typhoid Fever Prevalence In Bauchi North, Bauchi State, Nigeria. Dutse J of Pure and Applied Sci (DUJOPAS), 11 (2a): 158-168. https://dx.doi.org/10.4314/dujopas.v11i2a.14
Morgenstern, R., & Hayes, P. C. (1991). The liver in typhoid fever: always affected, not just a complication. Am J Gastroenterol, 86(9), 1235-1239.
Muhammad, H. L., Garba, R., Abdullah, A. S., Muhammad, H. K., Busari, M. B., Hamzah, R. U., & Makun, H. A. (2021). In vivo anti-typhoid and safety evaluation of extracts of Ximenia americana on experimental rats. Pharmacological Research - Modern Chinese Medicine, 1, 100009. https://doi.org/https://doi.org/10.1016/j.prmcm.2021.100009
Musa, T. H., Bello, A., Ahmed, Z., Garba, U., Sani, K., & Umar, Y., (2022). Typhoid fever prevalence in Bauchi State, Nigeria. Journal of Public Health Epidemiology, 14(1), 1–8
Natheua, C. K., Solange, D., Sylvie, N. O. & Bruno, P. T. (2020) Liver and Kidney Biochemical Profile of Typhoid Fever Patients at the Dschang District Hospital, West Cameroon: A Cross-Sectional Study. American Scientific Research Journal for Engineering, Technology, and Sciences (ASRJETS), 65(1), 149-162
Ndako, J. A., Dojumo, V. T., Akinwumi, J. A., Fajobi, V. O., Owolabi, A. O., & Olatinsu, O. (2020). Changes in some haematological parameters in typhoid fever patients attending Landmark University Medical Center, Omuaran-Nigeria. Heliyon, 6(5), e04002. https://doi.org/10.1016/j.heliyon.2020.e04002
Ndukaku, O. Y., Emmanuel, E. U., Mercy, E. A., & Caroline, N. O. (2015). Evaluation of the serum liver enzymes markers, lipid profile and kidney function parameters in typhoid patients. International J of Trop Dis & Health, 8(2), 79-89.
https://doi.org/10.9734/IJTDH/2015/17322
Ochiai, R. L., Acosta, C. J., Danovaro-Holliday, M. C., Baiqing, D., Bhattacharya, S. K., Agtini, M. D., . . . Clemens, J. D. (2008). A study of typhoid fever in five Asian countries: disease burden and implications for controls. Bull World Health Organ, 86(4), 260-268. https://doi.org/10.2471/blt.06.039818
Ohta, R., Tsumura, K. & Sano C. The Relationship Between Hyperalbuminemia and Unscheduled Medical Visits: A Retrospective Cohort Study. Cureus. 2024 Jul 28;16(7):e65585. doi: https://doi.org/10.7759/cureus.65585
Osu, M.U., Achov, V.O., Ashigabu, T.J., Hussaini, F.A., & Dawar, H.I. (2024) Epidemiology and Risk Factors for Endemic Typhoid Fever in Keffi Metropolis of Nasarawa State. Int Jr Infect Dis & Epidemlgy. 2024;5(2):1-10.
https://doi.org/10.51626/ijeti.2024.05.00077
Pancharoen, C., Wongsawat, J., Phancharoen, S., & Thisyakorn, U. (2001). Typhoid glomerulonephritis in a child: a rare complication of typhoid fever. Southeast Asian J Trop Med Public Health, 32(4), 869-871.
Qamar, U., & Aijaz, J. (2013). Haematological changes associated with typhoid fever. Rawal Med J, 38(1), 32-35.
Rajput, R., Jain, D., Kumar, A., & Mittal, A. (2016). Typhoid Fever Presenting With Acute Renal Failure And Hepatitis Simultaneously - A Rare Presentation. ARS Medica Tomitana, 22(2), 80-82. https://doi.org/doi:10.1515/arsm-2016-0014
Ratnayake, E. C., Shivanthan, C., & Wijesiriwardena, B. C. (2011). Cholestatic hepatitis in a patient with typhoid fever - a case report. Ann Clin Microbiol Antimicrob, 10, 35. https://doi.org/10.1186/1476-0711-10-35
Ringoringo, H. P., Wahyuni, I. I., Panghiyangani, R., Hartoyo, E., & Lao, R. (2022). Hematological profile of children under five years with typhoid fever at Idaman Banjarbaru Hospital, Indonesia. Bali Medical Journal, 11(2), 775-778. https://doi.org/10.21203/rs.3.rs-524279/v1
Seratin, F., Widiasta, A., Adrizain, R., & Hilmanto, D. (2022). An evaluation of kidney dysfunction as a common symptom of typhoid infection in an endemic country: A rare case study. IDCases, 29, e01580. https://doi.org/10.1016/j.idcr.2022.e01580
Shamim, A., Shamim, A ,&Hussain, B. (2012). Study of Biochemical Changes and Elevated Levels of Enzymes in Salmonella typhi Infected Patients in Pakistani Population. Int. J. Bioautomation, 16(1), 33-42
Shrivastava, K., Vahikar, S., & Mishra, V. (2015). Hematological profile in typhoid fever. Trop J Pathol Microbiol, 1(01). https://doi.org/10.17511/jopm.2015.i01.04
Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: Pathogenesis and Clinical Significance. JPEN J Parenter Enteral Nutr. 2019 Feb;43(2):181-193. https://doi.org/10.1002/jpen.1451
Vaishnavi, C., Singh, S., Kochhar, R., Bhasin, D., Singh, G., & Singh, K. (2005). Prevalence of Salmonella enterica serovar typhi in bile and stool of patients with biliary diseases and those requiring biliary drainage for other purposes. Jpn J Infect Dis, 58(6), 363-365. https://doi.org/10.7883/yoken.JJID.2005.363
Wain, J., Hendriksen, R. S., Mikoleit, M. L., Keddy, K. H., & Ochiai, R. L. (2015). Typhoid fever. Lancet, 385(9973), 1136-1145. https://doi.org/10.1016/s0140-6736(13)62708-7
Wankasi, M. M., George, G. S., Alabrah, P. W. & Agoro, E. S. (2022). Evaluation of Some Hepato-Renal Biochemical Parameters in Typhoid Fever Patients in Yenagoa, Bayelsa State Nigeria. Int J of TROPI Dis & Health. 43(14): 8-14. https://doi.org/10.9734/IJTDH/2022/v43i1430639
Wang, J., Ma, S., Li, W., Wang, X., Huang, D., Jiang, L., & Feng, L. (2021). Salmonella enterica Serovar Typhi Induces Host Metabolic Reprogramming to Increase Glucose Availability for Intracellular Replication. Int J Mol Sci, 22(18). https://doi.org/10.3390/ijms221810003
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Johnson Ojo Rotimi, Modupeoluwa Ogunfowokan Ifeoluwapo

This work is licensed under a Creative Commons Attribution 4.0 International License.