HEPATOPROTECTIVE AND NEPHROPROTECTIVE EFFECTS OF TOFACITINIB AND ASPIRIN AS ANTI-INFLAMMATORY DRUGS TARGETING JAK-STAT AND NF-κB SIGNALING PATHWAYS IN TYPE 2 DIABETES-INDUCED RATS.
DOI:
https://doi.org/10.33003/fjs-2025-0912-4119Keywords:
Complications, Hepatotoxicity, Inflammation, Nephrotoxicity, Type 2 DiabetesAbstract
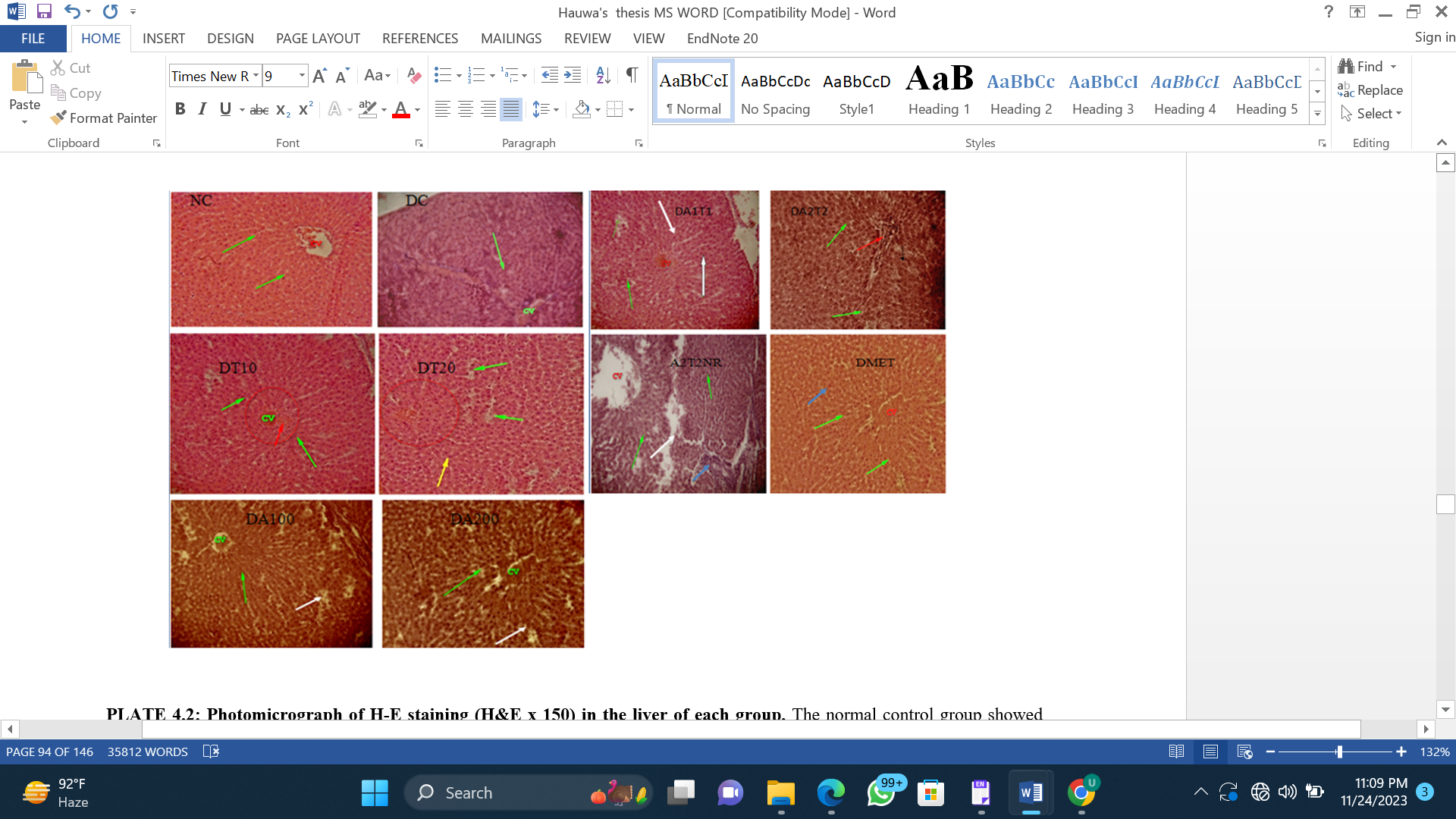
Chronic inflammation contributes to hepatic and renal complications in type 2 diabetes, largely through dysregulation of the JAK–STAT and NF-κB signaling pathways. This study evaluated the hepatoprotective and nephroprotective effects of tofacitinib (JAK–STAT inhibitor) and aspirin (NF-κB inhibitor) in streptozotocin-induced type 2 diabetic rats. Type 2 diabetes was induced using streptozotocin. Diabetic rats were treated orally with tofacitinib (10 or 20 mg/kg), aspirin (100 or 200 mg/kg), or combination therapy for 9 weeks. Serum ALT, AST, creatinine, and urea levels were quantified, and liver and kidney tissues were examined histologically. Statistical significance was set at P < 0.05. Diabetic controls showed substantial increases in ALT (74.56 ± 4.71 U/L), AST (181.30 ± 16.91 U/L), creatinine (45.33 ± 2.17 mg/dL), and urea (198.25 ± 6.49 mg/dL). Tofacitinib significantly reduced ALT to 32.32 ± 4.22 and 33.07 ± 4.06 U/L, AST to 79.80 ± 7.38 and 74.67 ± 6.37 U/L, creatinine to 17.25 ± 1.26 and 10.38 ± 1.02 mg/dL, and urea to 91.07 ± 9.48 and 61.36 ± 5.99 mg/dL at 10 and 20 mg/kg, respectively (P < 0.05). Aspirin at 100 mg/kg produced comparable improvements, while 200 mg/kg aspirin and combination regimens failed to significantly improve biomarkers (P > 0.05). Histopathology confirmed reduced hepatocyte degeneration and glomerular injury in effective treatment groups. In conclusion, tofacitinib and low-dose aspirin independently confer significant hepatoprotective and nephroprotective effects in type 2 diabetic rats, whereas combined therapy provides no added benefit.
References
Adelakun, S. A., Akomaye, A. J., Omotoso, O. D., & Arowosegbe, O. A. (2024). Anti-hepatopathy and anti-nephropathy activities of Taraxacum officinale in a rat model of Streptozotocin diabetes-induced hepatorenal toxicity and dyslipidemia via attenuation of oxidative stress, inflammation, apoptosis, electrolyte imbalances, and mitochondrial dysfunction. Aspects of Molecular Medicine, 3, 100034. https://doi.org/https://doi.org/10.1016/j.amolm.2024.100034
Adiga, U. S., & Malawadi, B. N. (2016). Association of Diabetic Nephropathy and Liver Disorders. J Clin Diagn Res, 10(10), Bc05-bc07. https://doi.org/10.7860/jcdr/2016/21672.8728
Arigela, C. S., Nelli, G., Gan, S. H., Sirajudeen, K. N. S., Krishnan, K., Abdul Rahman, N., & Pasupuleti, V. R. (2021). Bitter Gourd Honey Ameliorates Hepatic and Renal Diabetic Complications on Type 2 Diabetes Rat Models by Antioxidant, Anti-Inflammatory, and Anti-Apoptotic Mechanisms. Foods, 10(11), 2872. https://www.mdpi.com/2304-8158/10/11/2872
Ashoori, M., Bathaie, S. Z., & Heidarzadeh, H. (2015). Long-term, high-dose aspirin therapy increases the specific activity of complex III of mitochondrial respiratory chain in the kidney of diabetic rats. Physiology and Pharmacology, 19, 158-167.
Bako, H. Y., Ibrahim, M. A., Isah, M. S., & Ibrahim, S. (2019). Inhibition of JAK-STAT and NF-κB signalling systems could be a novel therapeutic target against insulin resistance and type 2 diabetes. Life Sci, 239, 117045. https://doi.org/10.1016/j.lfs.2019.117045
Cade, W. T. (2008). Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther, 88(11), 1322-1335. https://doi.org/10.2522/ptj.20080008
Cerf, M. E. (2013). Beta cell dysfunction and insulin resistance. Front Endocrinol (Lausanne), 4, 37. https://doi.org/10.3389/fendo.2013.00037
Chan, J. C. N., Lim, L. L., Wareham, N. J., Shaw, J. E., Orchard, T. J., Zhang, P., Lau, E. S. H., Eliasson, B., Kong, A. P. S., Ezzati, M., Aguilar-Salinas, C. A., McGill, M., Levitt, N. S., Ning, G., So, W. Y., Adams, J., Bracco, P., Forouhi, N. G., Gregory, G. A., Guo, J., Hua, X., Klatman, E. L., Magliano, D. J., Ng, B. P., Ogilvie, D., Panter, J., Pavkov, M., Shao, H., Unwin, N., White, M., Wou, C., Ma, R. C. W., Schmidt, M. I., Ramachandran, A., Seino, Y., Bennett, P. H., Oldenburg, B., Gagliardino, J. J., Luk, A. O. Y., Clarke, P. M., Ogle, G. D., Davies, M. J., Holman, R. R., & Gregg, E. W. (2021). The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet, 396(10267), 2019-2082. https://doi.org/10.1016/s0140-6736(20)32374-6
Galicia-Garcia, U., Benito-Vicente, A., Jebari, S., Larrea-Sebal, A., Siddiqi, H., Uribe, K. B., Ostolaza, H., & Martín, C. (2020). Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci, 21(17). https://doi.org/10.3390/ijms21176275
Isaacs, J. D., Zuckerman, A., Krishnaswami, S., Nduaka, C., Lan, S., Hutmacher, M. M., Boy, M. G., Kowalski, K., Menon, S., & Riese, R. (2014). Changes in serum creatinine in patients with active rheumatoid arthritis treated with tofacitinib: results from clinical trials. Arthritis Res Ther, 16(4), R158. https://doi.org/10.1186/ar4673
Islam, M. S. (2011). Fasting blood glucose and diagnosis of type 2 diabetes. Diabetes Res Clin Pract, 91(1), e26. https://doi.org/10.1016/j.diabres.2010.09.035
Kremer, J. M., Kivitz, A. J., Simon-Campos, J. A., Nasonov, E. L., Tony, H. P., Lee, S. K., Vlahos, B., Hammond, C., Bukowski, J., Li, H., Schulman, S. L., Raber, S., Zuckerman, A., & Isaacs, J. D. (2015). Evaluation of the effect of tofacitinib on measured glomerular filtration rate in patients with active rheumatoid arthritis: results from a randomised controlled trial. Arthritis Res Ther, 17(1), 95. https://doi.org/10.1186/s13075-015-0612-7
Kumar Bhatt, L., & Addepalli, V. (2011). Minocycline with aspirin: an approach to attenuate diabetic nephropathy in rats. Ren Fail, 33(1), 72-78. https://doi.org/10.3109/0886022x.2010.528117
Li, C. J., Yang, Z. H., Shi, X. L., & Liu, D. L. (2017). Effects of aspirin and enoxaparin in a rat model of liver fibrosis. World J Gastroenterol, 23(35), 6412-6419. https://doi.org/10.3748/wjg.v23.i35.6412
Magliano, D. J., Boyko, E. J., & committee, I. D. F. D. A. t. e. s. (2021). IDF Diabetes Atlas. In Idf diabetes atlas. International Diabetes Federation, 2021.
Palipoch, S., & Punsawad, C. (2013). Biochemical and histological study of rat liver and kidney injury induced by Cisplatin. J Toxicol Pathol, 26(3), 293-299. https://doi.org/10.1293/tox.26.293
Phaniendra, A., Jestadi, D. B., & Periyasamy, L. (2015). Free radicals: properties, sources, targets, and their implication in various diseases. Indian J Clin Biochem, 30(1), 11-26. https://doi.org/10.1007/s12291-014-0446-0
Sun, H., Saeedi, P., Karuranga, S., Pinkepank, M., Ogurtsova, K., Duncan, B. B., Stein, C., Basit, A., Chan, J. C., & Mbanya, J. C. (2022). IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes research and clinical practice, 183, 109119.
Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., Abbasi-Kangevari, M., Abbastabar, H., Abd-Allah, F., & Abdelalim, A. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204-1222.
Wang, H., Feng, X., Han, P., Lei, Y., Xia, Y., Tian, D., & Yan, W. (2019). The JAK inhibitor tofacitinib ameliorates immune‑mediated liver injury in mice. Mol Med Rep, 20(6), 4883-4892. https://doi.org/10.3892/mmr.2019.10750
Wesolowska-Andersen, A., Brorsson, C. A., Bizzotto, R., Mari, A., Tura, A., Koivula, R., Mahajan, A., Vinuela, A., Tajes, J. F., Sharma, S., Haid, M., Prehn, C., Artati, A., Hong, M.-G., Musholt, P. B., Kurbasic, A., De Masi, F., Tsirigos, K., Pedersen, H. K., Gudmundsdottir, V., Thomas, C. E., Banasik, K., Jennison, C., Jones, A., Kennedy, G., Bell, J., Thomas, L., Frost, G., Thomsen, H., Allin, K., Hansen, T. H., Vestergaard, H., Hansen, T., Rutters, F., Elders, P., t’Hart, L., Bonnefond, A., Canouil, M., Brage, S., Kokkola, T., Heggie, A., McEvoy, D., Hattersley, A., McDonald, T., Teare, H., Ridderstrale, M., Walker, M., Forgie, I., Giordano, G. N., Froguel, P., Pavo, I., Ruetten, H., Pedersen, O., Dermitzakis, E., Franks, P. W., Schwenk, J. M., Adamski, J., Pearson, E., McCarthy, M. I., & Brunak, S. (2022). Four groups of type 2 diabetes contribute to the etiological and clinical heterogeneity in newly diagnosed individuals: An IMI DIRECT study. Cell Reports Medicine, 3(1), 100477. https://doi.org/https://doi.org/10.1016/j.xcrm.2021.100477
World Health Organisation (2024). Health Topic on Diabetes 2024
Wu, T., Ding, L., Andoh, V., Zhang, J., & Chen, L. (2023). The Mechanism of Hyperglycemia-Induced Renal Cell Injury in Diabetic Nephropathy Disease: An Update. Life (Basel), 13(2). https://doi.org/10.3390/life13020539
Zhang, X., Lin, L., Li, L., Hu, K., Shao, R., Li, P., Tang, L., Zhu, M., Ma, Y., & Yang, Y. (2022). Janus kinase inhibitor Tofacitinib alleviated acute hepatitis induced by lipopolysaccharide/D-galactosamine in mice. Molecular Biology Reports, 50, 1-9. https://doi.org/10.1007/s11033-022-08086-6
Zhu, Y., Su, Y., Zhang, J., Zhang, Y., Li, Y., Han, Y., Dong, X., Li, W., & Li, W. (2021). Astragaloside IV alleviates liver injury in type 2 diabetes due to promotion of AMPK/mTOR‑mediated autophagy. Mol Med Rep, 23(6), 437. https://doi.org/10.3892/mmr.2021.12076
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 HAUWAU YAKUBU BAKO, Mohammed Auwal Ibrahim, Sani Ibrahim

This work is licensed under a Creative Commons Attribution 4.0 International License.