PREDICTIVE MODELING OF COVID-19 OUTBREAKS USING LOGISTIC REGRESSION AND DECISION TREE
DOI:
https://doi.org/10.33003/fjs-2025-0912-4206Keywords:
COVID-19, Decision Tree, Forecasting, Logistic Regression, Outbreak, Predictive Modeling, Public HealthAbstract
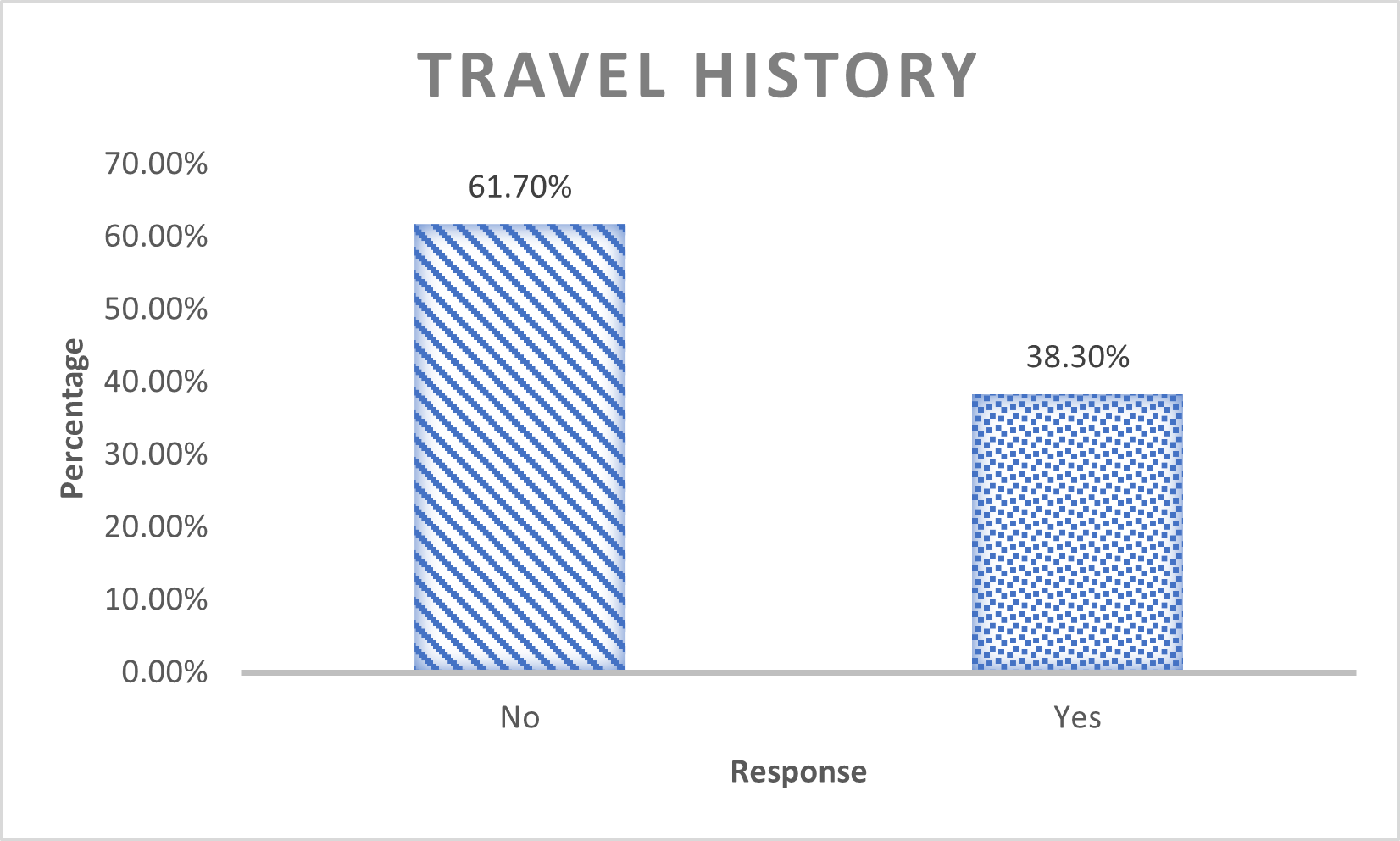
The COVID-19 pandemic caused by SARS-CoV-2 remains one of the most significant global health crises of the 21st century. This study focuses on modeling and predicting COVID-19 outbreak trends in Ebonyi State, Nigeria, using logistic regression and decision tree algorithms. Secondary data were sourced from the Nigeria Centre for Disease Control (NCDC), WHO COVID-19 Dashboard, and Google Mobility Reports. Sociodemographic variables, clinical symptoms, and exposure histories were analyzed to determine their influence on infection risk. Findings revealed that age, religion, marital status, educational level, and occupation were significant predictors of infection (p < 0.001), whereas gender and ethnicity were not. Marital status emerged as a strong independent predictor—single and divorced individuals were more likely to test positive compared to married individuals. Interestingly, individuals with a history of travel or contact with confirmed cases were less likely to test positive, suggesting behavioral adaptations following exposure. The study concludes that predictive modeling can support early detection, efficient resource allocation, and targeted interventions in public health.
References
Adebisi, Y. A., Rabe, A., and Lucero-Prisno, D. E. (2020). COVID-19 surveillance systems in Nigeria: Lessons and recommendations. Pan African Medical Journal, 35(Supp 2), 1–5. https://doi.org/10.11604/pamj.supp.2020.35.2.23267
Adegboye, O. A., Adekunle, A. I., and Gayawan, E. (2020). Early transmission dynamics of novel coronavirus (COVID-19) in Nigeria. International Journal of Environmental Research and Public Health, 17(9), 3054. https://doi.org/10.3390/ijerph17093054
Bassey, G., Akpan, B., and Etuk, I. (2021). Sociodemographic determinants of COVID-19 infection in Nigeria: A multicenter analysis. Nigerian Journal of Clinical Practice, 24(6), 889–896. https://doi.org/10.4103/njcp.njcp_89_21
Bi, Q., Wu, Y., Mei, S., Ye, C., Zou, X., Zhang, Z., ...and Feng, T. (2020). Epidemiology and transmission of COVID-19 in 391 cases and 1,286 of their close contacts in Shenzhen, China. The Lancet Infectious Diseases,20(8), 911–919. https://doi.org/10.1016/S1473-3099(20)30287-5
Carfì, A., Bernabei, R.,and Landi, F. (2020). Persistent symptoms in patients after acute COVID-19. JAMA, 324(6), 603–605. https://doi.org/10.1001/jama.2020.12603
Dagan, N., Barda, N., Kepten, E., Miron, O., Perchik, S., Katz, M. A., ...and Balicer, R. D. (2021). BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. New England Journal of Medicine, 384(15), 1412–1423. https://doi.org/10.1056/NEJMoa2101765
Gupta, A., Madhavan, M. V., Sehgal, K., Nair, N., Mahajan, S., Sehrawat, T. S., ...and Mehta, P. K. (2020). Extrapulmonary manifestations of COVID-19. Nature Medicine, 26(7), 1017–1032. https://doi.org/10.1038/s41591-020-0968-3
Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., ...and Zhong, N. S. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine, 382(18), 1708–1720. https://doi.org/10.1056/NEJMoa2002032
Iwuoha, V. C., Eze, C. J., and Nwankwo, C. F. (2021). Sociodemographic predictors of COVID-19 infection in South-East Nigeria. Journal of Infectious Diseases and Epidemiology, 7(204), 1–7. https://doi.org/10.23937/2474-3658/1510204
Kuhe, D. A., Udoumoh, . E. F. . ., and Ibeajaa, . U. L (2024). Modeling Novel Covid-19 Pandemic in Nigeria Using Count Data Regression Models. Fudma Journal OF SCIENCES, 8(1), 111-117. https://doi.org/10.33003/fjs-2024-0801-2211
Kucharski, A. J., Russell, T. W., Diamond, C., Liu, Y., Edmunds, J., Funk, S., ...and Eggo, R. M. (2020). Early dynamics of transmission and control of COVID-19: A mathematical modelling study. The Lancet Infectious Diseases, 20(5), 553–558. https://doi.org/10.1016/S1473-3099(20)30144-4
Kumar, D.,and Malviya, R. (2020). Corona virus: A review of COVID-19. Eurasian Journal of Medicine and Oncology, 4(1), 8–25. https://doi.org/10.14744/ejmo.2020.51418
Lechien, J. R., Chiesa-Estomba, C. M., De Siati, D. R., Horoi, M., Le Bon, S. D., Rodriguez, A., and Dequanter, D. (2020). Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate COVID-19: A multicenter European study. European Archives of Oto-Rhino-Laryngology, 277(8), 2251–2261. https://doi.org/10.1007/s00405-020-05965-1
Liu, Y., Gayle, A. A., Wilder-Smith, A.,and Rocklöv, J. (2020). The reproductive number of COVID-19 is higher compared to SARS coronavirus. Journal of Travel Medicine, 27(2), taaa021. https://doi.org/10.1093/jtm/taaa021
Nouvellet, P., Bhatia, S., Cori, A., Ainslie, K. E. C., Baguelin, M., Bhatt, S., ...and Ferguson, N. M. (2021). Reduction in mobility and COVID-19 transmission. Nature Communications, 12, 1090. https://doi.org/10.1038/s41467-021-21358-2
NCDC. (2020). First confirmed case of COVID-19 in Nigeria. Nigeria Centre for Disease Control. https://ncdc.gov.ng/news
Ogundokun, R. O., Awotunde, J. B., and Yalogun, G. (2021). Predictive modeling of COVID-19 spread in Nigeria using machine learning techniques. Informatics in Medicine Unlocked, 23, 100515. https://doi.org/10.1016/j.imu.2021.100515
Okoro, N., and Taiwo, A. (2021). Ethnicity, social inequality, and COVID-19 outcomes in Nigeria. African Population Studies, 35(1), 5782–5794. https://doi.org/10.11564/35-1-1580
Onyema, E. M., Nwodo, A. N., and Mbah, P. O. (2021). Public awareness, behavior change, and COVID-19 preventive practices in Nigeria. Cogent Social Sciences, 7(1), 1942061. https://doi.org/10.1080/23311886.2021.1942061
Otu, A., Charles, C., and Yaya, S. (2020). COVID-19 symptoms and comorbidities in Nigerian patients: A retrospective clinical analysis. The Pan African Medical Journal, 35(Supp 2), 1–7. https://doi.org/10.11604/pamj.supp.2020.35.2.23278
Ukpong, E. E., Effiong, A. I., and Udo, U. E. (2021). Sociocultural factors and COVID-19 infection patterns in Nigeria. Journal of Public Health in Africa, 12(s1), 1–9. https://doi.org/10.4081/jphia.2021.1764
Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., and Zhao, Y. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA, 323(11), 1061–1069. https://doi.org/10.1001/jama.2020.1585
Wiersinga, W. J., Rhodes, A., Cheng, A. C., Peacock, S. J.,and Prescott, H. C. (2020). Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19). JAMA, 324(8), 782–793. https://doi.org/10.1001/jama.2020.12839
World Health Organization. (2021). WHO COVID-19 global epidemiological updates. https://www.who.int
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., ...and McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. https://doi.org/10.1016/j.jad.2020.08.001
Zhou, P., Yang, X. L., Wang, X. G., Hu, B., Zhang, L., Zhang, W., ...and Shi, Z. L. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), 270–273. https://doi.org/10.1038/s41586-020-2012-7
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Stephen O. Etebefia, Victor Obukohwo, Chidinma A. Ibegbulam

This work is licensed under a Creative Commons Attribution 4.0 International License.